February 18, 2026
Optum uses AI to drive affordability and accelerate value-based care adoption
Value Connect turns real-time insight into action to support healthier lives, with on average 35% lower medical spend and 20%+ improvement in care gap closure.
(Feb. 18, 2026) As the health care industry moves toward value-based — or preventative, integrated care — one key insight has become clear: the model cannot succeed without the right infrastructure to support it. Payers and providers continue to face fragmented data, disconnected workflows and administrative hurdles that make it difficult to align decisions and deliver better outcomes. These gaps make it hard for even the most promising programs to succeed.
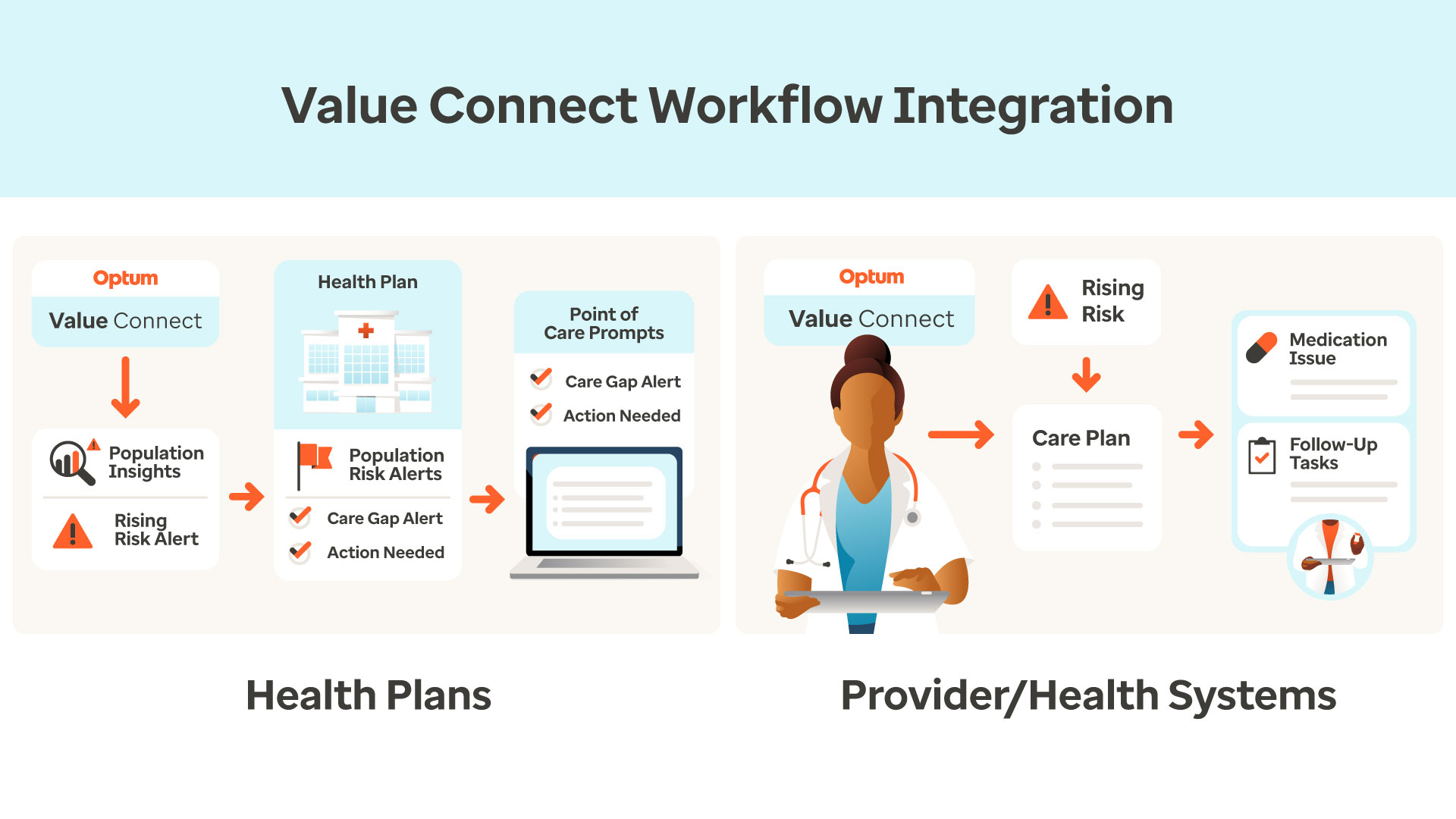
Optum is addressing these challenges through Value Connect, an AI-powered platform that helps organizations act on insight, not just interpret it. Value Connect unifies clinical, operational, and financial capabilities into a shared platform that enables payers and providers to more holistically understand the populations they serve, help prioritize intervention strategies, and drive action that helps both improving member health and reducing the total cost of care.
“We’re accelerating the shift to value-based care by meeting payers and providers where they are in their journey,” said Beth Merle, senior vice president, Provider Enablement at Optum Insight. “The solution empowers organizations to proactively manage risk and costs while improving outcomes for the people they serve.”
AI that supports proactive care strategies
Value Connect applies AI across quality measures, utilization patterns, and risk indicators to identify who needs support and where action will have the greatest impact. Optum’s award‑winning GenAI analyzes the data at scale and powers more than 1,600 models. Insights such as early disease detection are translated into clear next steps and priorities for care teams to leverage in their decision making.
Operationalizing insight at the point of care
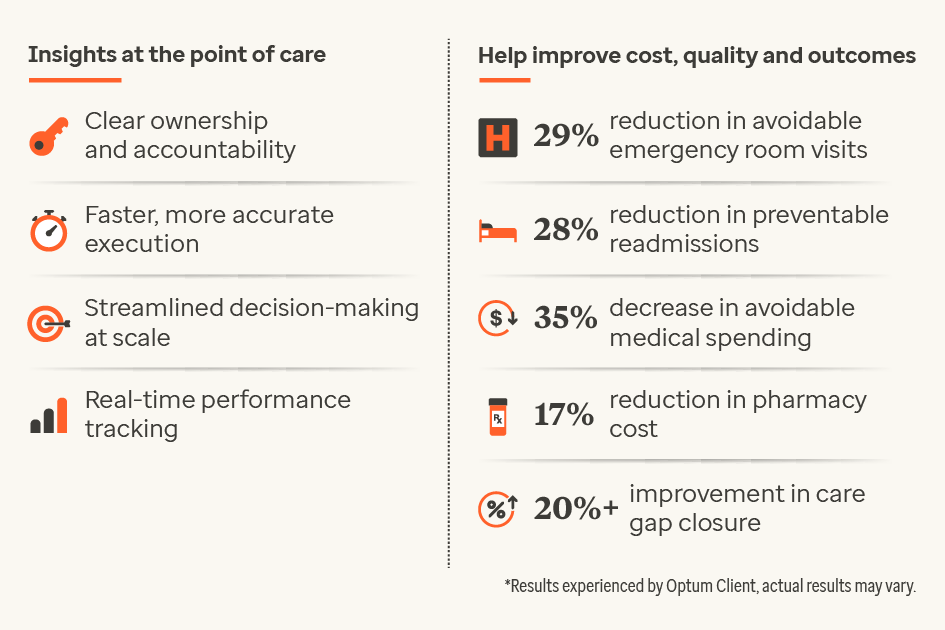
Despite 75% of health system executives prioritizing digital and analytics transformation, many organizations don’t have the tools to act on insights. Value Connect eliminates the need for spreadsheets and handoffs by routing actionable steps directly into workflows, resulting in faster execution, clearer ownership, and consistent progress tracking. Access to earlier insights help payers improve member health and reduce avoidable costs.
Direct impact on affordability, quality, and health outcomes
Payers and providers using Value Connect capabilities are already seeing meaningful improvements. On average, our customers are seeing a 29% reduction in emergency room visits and a 28% reduction in preventable hospital readmissions. Medical spending has dropped 35% and pharmacy costs by 17%, contributing to a lower total costs of care. Additionally, care gap closure has increased by more than 20%, supporting improvements in quality and member experiences.
As an early adopter of Value Connect, Keck Medicine of USC is helping advance a shared commitment to better outcomes. “Our hope is that the collaboration with Optum will help us to accelerate the shift to value-based care,” said Rod Hanners, chief executive officer, Keck Medicine of USC. “By leveraging Optum’s Value Connect platform and advanced AI capabilities, we expect to be able to unify data, streamline workflows, and take timely action.”
Creating a sustainable future for health care
Optum is helping shape a future where insight-driven collaboration becomes the norm. For payers, this means healthier members, stronger networks and more predictable performance. For providers, this means simpler administration and improved patient outcomes. For communities, it means a health care system that supports greater affordability and is easier to navigate.